Breadcrumbs
Faculty Lead Updates
August 2023

Anne Matlow, MD, FRCPC, CEC
While the need for healthcare reform is readily evident to the general public, physicians and other healthcare workers are acutely aware of the challenges involved in providing safe, timely, effective and equitable healthcare that meets the needs of each individual patient. Physician leadership is essential at all levels of the system in order to optimize patient care.
Good leadership requires the exercising of a multitude of capabilities, influencing others toward a desired end. It has long been recognized that the capabilities of leadership can be learned, and like muscles they grow and evolve over time. These capabilities must be embedded within the fabric of medical education for learners to capitalize on every possible opportunity to enact them, and to appreciate their ability to make a difference throughout their career. Indeed the role of leader is inherent in both the CanMEDS and CanMEDS-FM competencies, and postgraduate training programs must cover the relevant competencies in their educational offerings.
Given the importance of grooming the healthcare leaders of today and tomorrow, PGME offers a number of leadership educational opportunities to complement existing curricula in the various training programs. Our PG Leadership Certificate Program (PGLC) is now in its fifth year, and to date over 100 postgraduate learners have partaken in the experience. The PGLC is a longitudinal programme in which participants benefit from lectures, interactive workshops and fireside chats with leaders in healthcare, and are responsible for developing and implementing an action learning project. This constitutes leadership in action and is one of the highlights of the program. Numerous projects have impacted educational curricula and patient care in novel and creative ways.
PGME also offers a series of 11 leadership topics that programs can select from our Leading By Example Educational (LBE) Series menu, for incorporation into academic half days and educational retreats. More than 25 workshops and presentations were invited from the LBE series this past academic year.
Fostering leaders and leadership extends beyond our offerings for learners. In keeping with institutional accreditation standards, we have scaled up our process for regular multi-source feedback for program directors, a process designed to provide a formative assessment of their performance to date in their role. We have also offered coaching as a resource to support program directors in their role, in acknowledgement of the important work they do.
PGME’s investment in leadership training reflects our commitment to our learners in preparing them to provide exemplary patient care and transform the healthcare system locally and/ or beyond. Our program directors are instrumental and key effectors in that regard. We continue to align our leadership offerings with the faculty’s current academic strategic plan, contributing to the goal of ‘Leadership in advancing new knowledge, better health and equity’.
Fellowship Tip: Utilize the PEAP Period to its Fullest Extent

John Granton, MD (Fellowship Lead)
Background
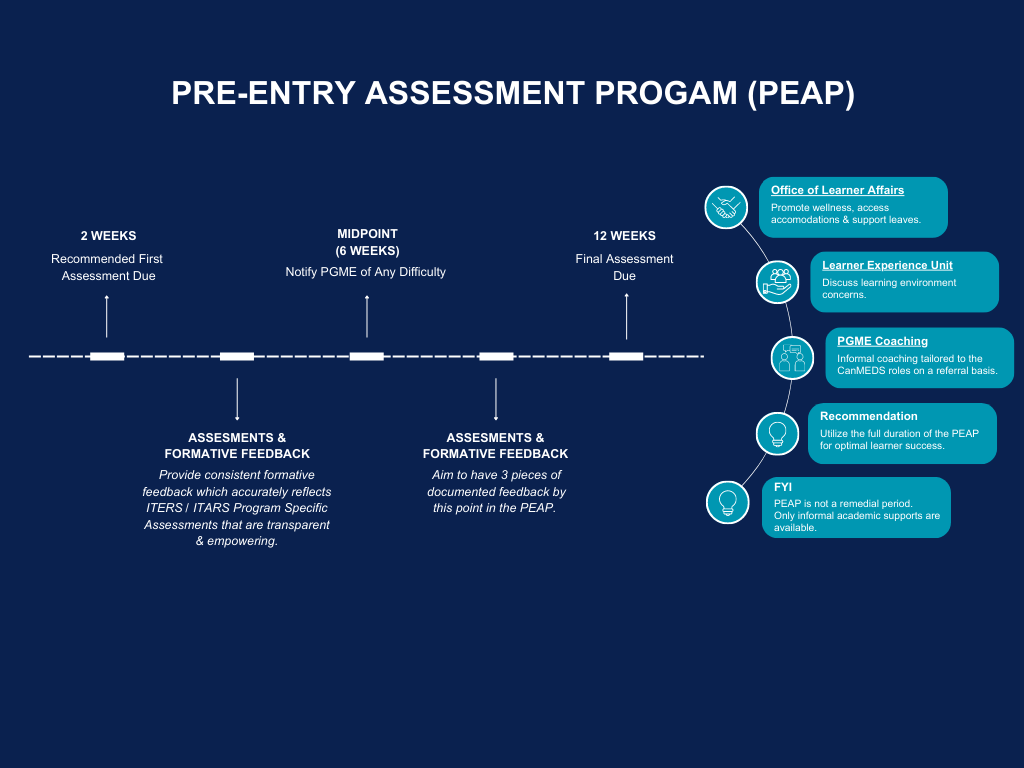
The Pre-Entry Assessment Program (PEAP) evaluates certified international medical graduates to determine their suitability for the designated level of training. To ensure a successful transition for all clinical fellows requiring a PEAP, we highly recommend that you:
1) Utilize the full 12-week duration of the PEAP. Although the minimum duration can be 4 weeks, we strongly recommend that the full 12-week period be utilized. This will allow time to fully assess competence (and document accordingly), provide feedback, and allow the fellow to address concerns in performance.
2) Provide consistent formative feedback. Feedback is integral to reinforce areas of strength as well as to address areas of concern. It will also ensure that issues around competence are documented early and that fellows in difficulty are flagged early to allow for additional supports to aid in this transition/assessment. Failure to document or inaccuracies lead to significant challenges if, at the end of the PEAP period, the fellow is felt to have not met an acceptable level of performance.
3) Contact PGME if you face any difficulties or there are concerns about the fellow’s performance. Please notify us at the midpoint (6-week mark) if you or any fellow is not progressing well. The Office of Learner Affairs is an excellent resource and is available to support clinical fellows in achieving academic and professional goals.
4) Submit the required evaluations to your Department Fellowship contact. The final evaluation form is mandatory and must be submitted five days prior to the PEAP end date; interim assessments with documented meetings are strongly recommended.
For more information please visit our FAQ on the PGME website.
Evaluate the fellow formally and regularly. Provide accurate, constructive feedback and document, document, document!

Petal Abdool, MD, FRCPC
As Faculty Lead for Simulation Education Integration, I was in awe of the depth and breadth of the Temerty Faculty of Medicine. I am eager to break down silos and build a Sim Community. It is a privilege to network with passionate Simulation Educators and Researchers across our Faculty and learn about their innovative work. We plan to use newsletters and Sim City Rounds as platforms to showcase Sim-related achievements and create opportunities to collaborate. Members of our Faculty are extremely busy making the world a better place so we have recorded our Sim City Rounds on YouTube to view at a convenient time. Here is the link to the playlist: Sim City Rounds
Please feel free to contact us at SimCitynews@utoronto.ca if you would like to share Sim related projects, publications or events.
VR Updates: CAMH Simulation Centre: VR Simulatoin of an Opiod Overdose

CAMH Sim Centre has designed a VR Opioid Overdose Training based on an identified gap/Needs Assessment. One source was PGME trainees at the Temerty Faculty of Medicine.
By the end of the VR Opioid Overdose simulation, learners will be able to:
- Assess a collapse for safety
- Identify an opioid overdose and call for help
- Administer the required treatment and monitor the patient’s response
- Support the patient after an overdose
Our target audience is:
- Clinicians, and clinicians in training, who work in community clinical settings/mental health facilities
- Any person who may respond to an overdose outside of a medical setting
UPCOMING SIMULATION-FOCUSED EVENTS
- SimGHOSTS USA 2023: August 1-4, 2023 | Omaha, Nebraska | website
- CAPE Simulation Instructor Program: August 14- 16, 2023 | Stanford, California | website
- IM Expo 2023: December 11-12, 2023 | Ottawa, Ontario | website
- Canadian Simulation Exchange Webinars: Monthly, beginning in September 2023. Email CanSimExchange@gmail.com to join the distribution list and for information to register for webinars.
TEMERTY FACULTY OF MEDICINE SIM PUBLICATIONS
Virtual Reality Simulation for Suicide Risk Assessment Training: Prevalence of Adverse Effects Bahadur, A. G., Hargreaves, F., Antinucci, R., Sockalingam, S., & Abdool, P. S. (2023).
Considerations for psychological safety with system-focused debriefings
Mirette Dube, David Kessler, Lennox Huang, Andrew Petrosoniak, and Komal Bajaj
Artificial Intelligence for Intraoperative Guidance: Using Semantic Segmentation to Identify Surgical Anatomy During Laparoscopic Cholecystectomy.
Amin Madani, Babak Namazi, Maria S. Altieri, Daniel A. Hashimoto, Angela Maria Rivera, Philip H. Pucher, Allison Navarrete-Welton, Ganesh Sankaranarayanan, L. Michael Brunt, Allan Okrainec, Adnan Alseidi
An Immersive Simulation to Build Empathy for Geriatric Patients with Co-Occurring Physical and Mental Illness.
Anika Saiva, Petal S. Abdool, Laura M. Naismith, Latika Nirula
NEXT SIM CITY ROUNDS: SEPTEMBER 7, 2023 | 12:00-1:00PM | ZOOM LINK

Translational simulation: Building Health Systems for the Future
Presenter: Andrew Petrosoniak, MD, MSc (MedEd), FRCPC Emergency Physician & Trauma Team Leader
Lead, Translational Simulation & Clinical Integration
St. Michael’s Hospital
Assistant Professor, University of Toronto
Associate Scientist, Li Ka Shing Knowledge Institute Co-Principal, Advanced Performance Healthcare Design

Nirit Bernhard MSC, MD, FRCPC
An emerging goal of health professions education is to develop reflective practitioners who can embody competence, compassion, collaboration and tolerance for ambiguity in the face of uncertainty (1). Clinicians who can interpret the meaning of events around them, and adjust their practice accordingly, have fewer difficulties in their careers with patients, colleagues, and regulatory bodies (2).
Recognition of the importance of reflection in clinical practice has spurred course development and has led to many courses around the world whose focus is to teach medical learners about reflective practice. At the Temerty Faculty of Medicine, Portfolio was initially developed over a decade ago in the MD Program. Portfolio gives MD students the opportunity to engage in reflective practice during their undergraduate medical program as they are developing into doctors. Rising from its success, several postgraduate programs have also developed reflective practice rounds for their trainees.

PGME Portfolio (PGPORT) was established in 2022 to create equal access to reflective opportunities across all PG programs by facilitating the dialogue and themes that transcend the many post-graduate programs and subspecialties at Temerty Medicine.
PGPORT can be brought into any of the Postgraduate programs using a handbook (toolkit) that outlines the curriculum and reviews the topics, companion pieces to help guide discussion, and prompts to elicit dialogue with the aim of promoting the development and honing of reflective skills in the post graduate learner. PGPORT draws on several evidence-based methods of reflective practice, including the Balint method and elements of COMPASS group (3,4). Unlike these specific methods, PGPORT allows for more structured meetings grounded by certain recurring themes that have been identified by residents in training. As the group evolves organically, members can challenge each other by delving into more specific cases that are unique and relevant to their specific program, as guided by the postgraduate learners themselves.
PGPORT aims to have fellow residents meet their colleagues in a psychologically safe environment which allows them to share and reflect on their experiences. These themes include topics such as patient safety, shame in medicine, ambiguity and the role of humility in medicine, the hidden curriculum and exploring the power dynamic, racism and hierarchies in medicine.
Why is it critical to create space in our curriculum for reflective practice? There is evidence to suggest that this process may lead to transformative changes in the learner, and that being a reflective practitioner can help mitigate burnout and promote physician wellbeing (5,6). The bottom line is that reflective practitioners make better, happier doctors and PGPORT hopes to be one tool, among many, to get post-graduate learners closer to that goal!
References:
- Roberts M. Balint groups: a tool for personal and professional resilience. Canadian family physician, 2012; 58(3), 245–247.
- Franco R, Giuliani dos Santos Franco C, Pestana O, Severo M and Ferreira MA (2017) The use of portfolios to foster professionalism: attributes, outcomes, and recommendations, Assessment & Evaluation in Higher Education, 42:5, 737-755
- Balint M. The doctor, his patient and the illness. London, UK: Churchill Livingstone; 1957.
- West, CP, Dyrbye LN, Satele DV, Shanfelt TD. Colleagues Meeting to Promote and Sustain Satisfaction for Physician Wellbeing: A Randomized Controlled Trial. Mayo Clin Proc 2021 Oct; 96 (10):2606-2614.
- Shapiro J, McDonald TB. Supporting Clinicians during Covid-19 and Beyond — Learning from Past Failures and Envisioning New Strategies NEJM October 14, 2020
- Kjeldmand D, Holmström I. Balint groups as a means to increase job satisfaction and prevent burnout among general practitioners. Ann Fam Med 2008;6(2):1. 20238-45.

Jennifer Croke, MD, MHPE, FRCPC
In May 2023, PGME implemented a Mentorship Program for New Program Directors of Royal College accredited programs that is led by Dr. Jennifer Croke. To date, we have created Mentorship Program resources, including a handbook, and held a virtual information session for potential mentors (Feb 2023), created 10 mentee-mentor dyads (April 2023), and conducted a virtual orientation session for these mentorship dyads (May 2023). Mentorship pairings will continue to be created as we receive information regarding new Program Directors. An evaluation of the pilot program is ongoing.
News


